Written by: Bianca Løge (she/her).
Edited by: Zahra Taboun (she/her).
I had no idea what the NuvaRing was when I was recommended it by the McGill Macdonald Campus Nurse. I had no other friends already using it and kept questioning how can something so easy to use be as effective? I had always assumed that the greater the hassle, the greater the protection. And how does it stay up there?
Despite my skepticism, I was willing to give it a try. I have now been using the NuvaRing for two years, and I am always surprised as to how few people know about this form of contraceptive. I am so happy with it, as it is the only form of birth control that really works for me, my lifestyle, my wallet, my body, and my health.
It is the only form of birth control that really works for me, my lifestyle, my wallet, my body, and my health.
My first few months using the NuvaRing I kept to the manual that it comes with. The instructions include a diagram of a person inserting the NuvaRing in all types of positions: laying down, standing up, squatting… similar to “how to insert a tampon” diagrams. Just like tampons, it is much easier than they make it look.
The NuvaRing is a small, flexible, plastic ring, the size of a hair tie, which releases 15 μg of ethinyl estradiol and 120 μg of etonogestrel per day over 3 consecutive weeks. Ethinyl estradiol works to prevent the release of the egg during the menstrual cycle, thickens vaginal fluid to prevent sperm from reaching the egg, and alters the lining of the uterus to prevent the attachment of a fertilized egg (1). Etonogestrel also increases vaginal fluid viscosity, alters the lining of the uterus, and inhibits the release of luteinizing hormone (LH), one of the reproductive hormones important in ovulation (2). The NuvaRing is easily self-inserted and left for three weeks before it is removed for one week. That’s right, I only have to worry about it two times a month!
After my first month of using it, I already recognized the many advantages to this form of birth control.
- It is easy to insert and remove. In a randomized multicenter, open-label, trial, 96% of individuals found NuvaRing easy to insert and 97% found it easy to remove (3).
- NuvaRing has comparable efficacy and tolerability with a combined oral contraceptive (COC) (4), and compliance (89.2% NuvaRing, 85.5% COC) and satisfaction (84% NuvaRing; 87% COC) were high and similar to COC (5)
- NuvaRing does not require daily dosing. It’s not the 5- or 10-year life of an IUD, but it also isn’t the daily dosing of a COC. I find the NuvaRing the goldilocks of birth control, as the perfect less invasive and lower maintenance alternative.
There are even more technical benefits of using the NuvaRing compared to other forms of birth control, mainly attributed to its lower dose of hormones. Compared with a COC containing 150 μg etonogestrel and 30 μg ethinyl estradiol, systemic exposure to etonogestrel is similar for NuvaRing, whereas systemic exposure to ethinyl estradiol with NuvaRing is approximately 50% of that of the COC (6), (7).
- NuvaRing uses a lower dose of contraceptive hormones, and its controlled-release delivery avoids daily fluctuations in hormone levels (8).
- The vaginal route of administration keeps the hormone absorption local which avoids hepatic first-pass metabolism and gastrointestinal interference with the absorption of hormones (8).
- When individuals who generally preferred oral contraceptives were introduced to the NuvaRing, after three cycles of ring use, 81% preferred the ring. On study completion:
- 97% agreed that the instructions for use were clear
- 85% of individuals and 71% of their partners never/rarely felt the ring during intercourse
- Overall acceptance was high, 96% were satisfied with the ring and 97% would recommend the ring (9)
- NuvaRing has excellent cycle control: breakthrough bleeding or spotting during cycles 2–13 was in general less frequent with NuvaRing than that with the COC (4.7–10.4%) (10), (11).
- Studies find improved cycle control and reduction in menorrhagia (long periods) and dysmenorrhea (painful periods) (12).
Although a large percentage preferred the ring, there are still individuals who did not. With the NuvaRing, there are similar estrogen-related adverse events as COCs, but users of the NuvaRing have also experienced more niche effects. Most are an increase of local adverse events such as leukorrhea, vaginal discomfort, vaginitis, and ring-related events comprising foreign body sensation, coital problems, and expulsions (13).
I understand the uncomfort of having a foreign substance in there, or the fear of it falling out, but this has not proved a barrier in my contraceptive use.
There is no idealized patient that the NuvaRing is particularly suited for, but rather it is highly acceptable among younger and older reproductive-age individuals regardless of how many children they had (14). Most of the studies around NuvaRing have only included cis-women, but it is important to acknowledge that it is not only for cis-women, despite the lack of research for individuals of other genders who have vaginas. For me, the NuvaRing costs 28.86 CAD for a pack of three in Quebec under RAMQ (Quebec health insurance plan). The ring’s cost can vary depending on province but ranges between 30-200$ a month without health insurance plans.
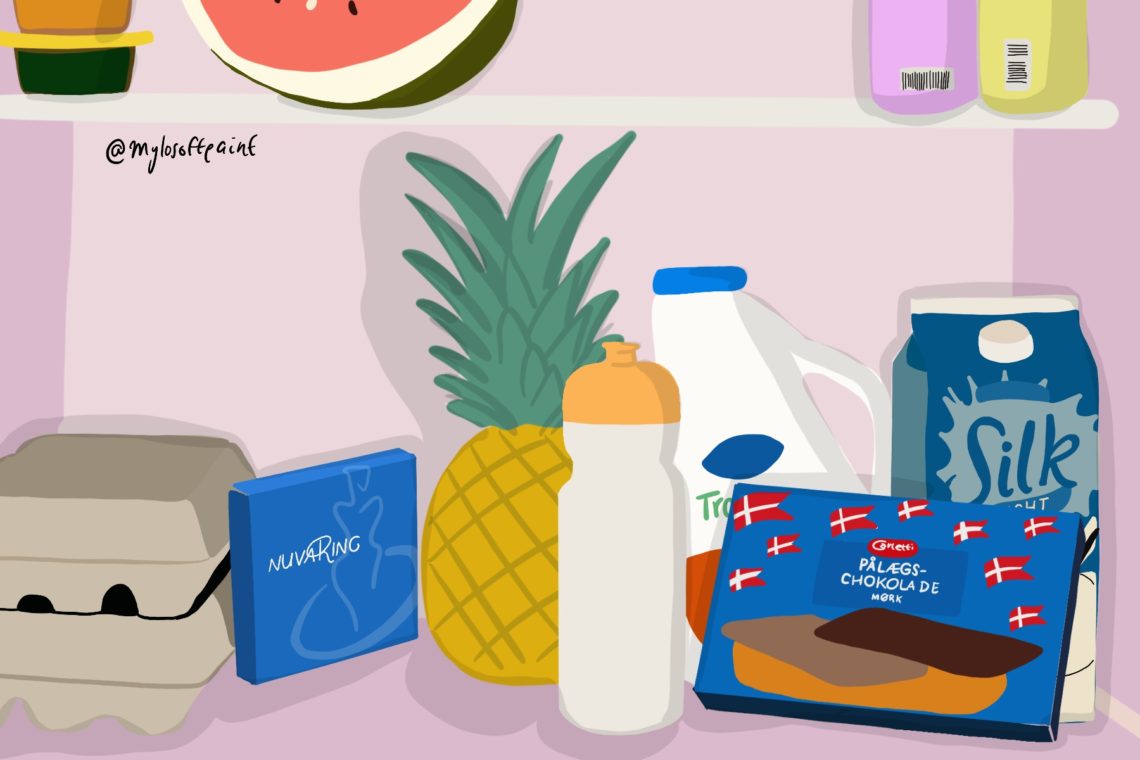
The NuvaRing also requires fridge-storage. When I moved to Denmark and put my blue NuvaRing box in my fridge, my Danish roommate became so excited when they saw the box, thinking it was a new type of Pålægschokolade: thin slices of chocolate that are used as a topping on bread, which also has a blue box (boxes compared below). Although the box needs to be kept in the fridge, it is so discrete and small to keep.
I understand that everyone has their own goldilocks of birth control, and this one is mine. I highly recommend it, and I believe that birth control should not be scary. Birth control should be as positive as Pålægschokolade.
References:
1. Keam S, Wagstaff A. Ethinylestradiol/Drospirenone. Treatments in Endocrinology. 2003;2(1):49-70.
2. Maddox D, Rahman Z. Etonogestrel (Implanon), Another Treatment Option for Contraception. Pharmacy and Therapeutics [Internet]. 2008 [cited 15 March 2021];33(6):337–347. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2683610/
3. Ahrendt H, Nisand I, Bastianelli C, Gómez M, Gemzell-Danielsson K, Urdl W et al. Efficacy, acceptability and tolerability of the combined contraceptive ring, NuvaRing, compared with an oral contraceptive containing 30 μg of ethinyl estradiol and 3 mg of drospirenone. Contraception. 2006;74(6):451-457.
4. Oddsson K, Leifels-Fischer B, de Melo N, Wiel-Masson D, Benedetto C, Verhoeven C et al. Efficacy and safety of a contraceptive vaginal ring (NuvaRing) compared with a combined oral contraceptive: a 1-year randomized trial. Contraception. 2005;71(3):176-182.
5. Ahrendt H, Nisand I, Bastianelli C, Gómez M, Gemzell-Danielsson K, Urdl W et al. Efficacy, acceptability and tolerability of the combined contraceptive ring, NuvaRing, compared with an oral contraceptive containing 30 μg of ethinyl estradiol and 3 mg of drospirenone. Contraception. 2006;74(6):451-457.
6. Timmer C, Mulders T. Pharmacokinetics of Etonogestrel and Ethinylestradiol Released from a Combined Contraceptive Vaginal Ring. Clinical Pharmacokinetics. 2000;39(3):233-242.
7. van den Heuvel M, van Bragt A, Alnabawy A, Kaptein M. Comparison of ethinylestradiol pharmacokinetics in three hormonal contraceptive formulations: the vaginal ring, the transdermal patch and an oral contraceptive. Contraception. 2005;72(3):168-174.
8. Timmer C, Mulders T. Pharmacokinetics of Etonogestrel and Ethinylestradiol Released from a Combined Contraceptive Vaginal Ring. Clinical Pharmacokinetics. 2000;39(3):233-242.
9. Novák A, de la Loge C, Abetz L, van der Meulen E. The combined contraceptive vaginal ring, NuvaRing®: an international study of user acceptability. Contraception. 2003;67(3):187-194.
10. Milsom I, Lete I, Bjertnaes A, Rokstad K, Lindh I, Gruber C et al. Effects on cycle control and bodyweight of the combined contraceptive ring, NuvaRing, versus an oral contraceptive containing 30 g ethinyl estradiol and 3 mg drospirenone. Human Reproduction. 2006;21(9):2304-2311.
11. Bjarnadóttir R, Tuppurainen M, Killick S. Comparison of cycle control with a combined contraceptive vaginal ring and oral levonorgestrel/ethinyl estradiol. American Journal of Obstetrics and Gynecology. 2002;186(3):389-395.
12. Wieder D. Examining the efficacy, safety, and patient acceptability of the combined contraceptive vaginal ring (NuvaRing®). International Journal of Women’s Health. 2010;:401.
13. Roumen F. Review of the combined contraceptive vaginal ring, NuvaRing<sup>®</sup>. Therapeutics and Clinical Risk Management. 2008;Volume 4:441-451.
14. Wieder D, Pattimakiel L. Examining the efficacy, safety, and patient acceptability of the combined contraceptive vaginal ring (NuvaRing®). International Journal of Women’s Health. 2010;2:401-409.