Written by: Helen Martin (she/her)
Edited by: Miles Llewellyn (they/them).
More and more young people are identifying as trans, non-binary, and gender non-conforming (TNBGN*). However, the biomedical approach commonly used in research and medical care for menstruation often overlooks the perspectives and preferences of TNBGN menstruators. As such, a literature review (see below) was conducted in order to synthesize the small body of research available on the preferences and experiences of TNBGN menstruators. As a result, we have been able to provide a set of nuanced recommendations to healthcare providers.
Unsurprisingly, prominent themes of the review included gender dysphoria, hormonal menstrual suppression, and the widespread controversy over bathroom access for TNBGN folks. However, this review also revealed important considerations specific to healthcare providers. While healthcare providers are still encouraged to enroll in formal training on how to deliver TNBGN care, the short-term recommendation for everyday medical practice can still make a meaningful difference to TNBGN patients.
Short-term Recommendations
- Update electronic medical records & paperwork systems to ensure all clinic staff consistently use the correct names, pronouns, and gender markers when conversing with patients.
- It is likely that when participants feel they and their gender identity are respected, they are also more inclined to access vital healthcare beyond gender-affirming care.
- Ask for consent to discuss menstruation – many patients may not want or need to discuss their menstruation. Some may have medically or surgically suppressed their menstruation long ago and these questions will likely feel irrelevant and non-affirming [1].
- Consider modifying electronic medical record systems so they no longer prompt practitioners to ask patients for their last menstrual cycle.
- Consider using more clinical terms instead of common terms which often have gendered connotations (“menstruation” and “menstrual product” instead of “period” or “tampon”) [1].
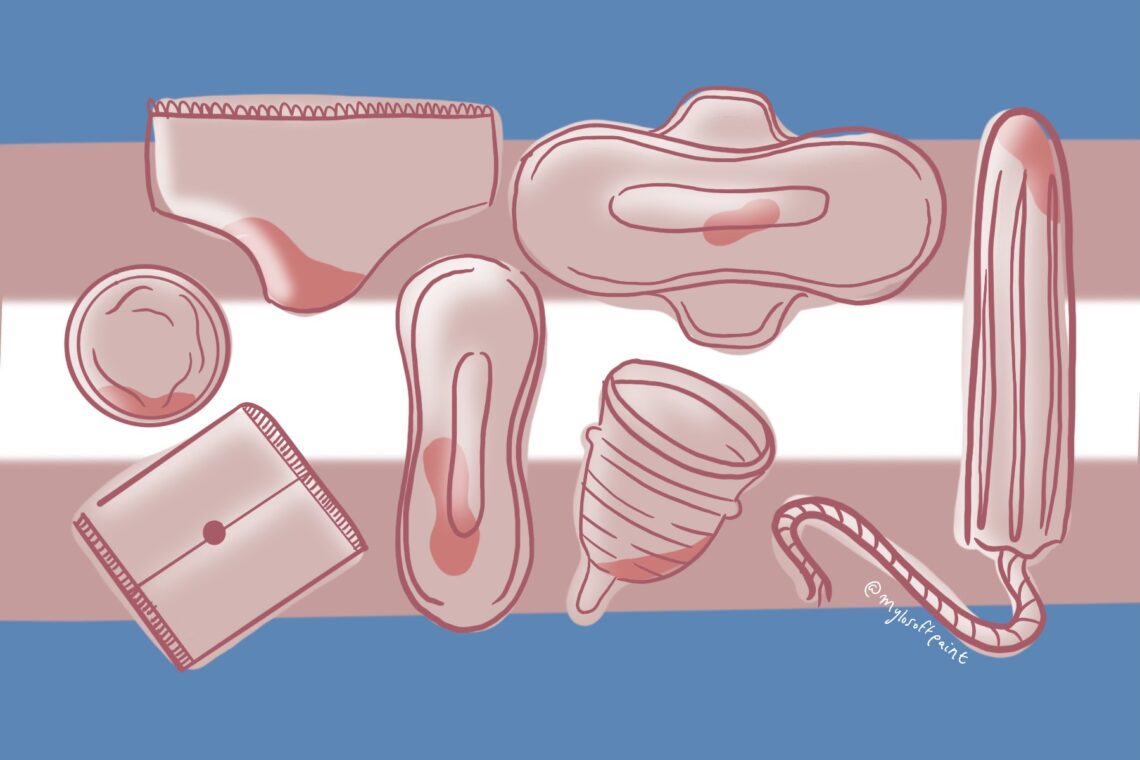
- TNBGN patients may be unaware of the variety of menstrual products available to them beyond tampons or pads, both of which may cause dysphoria [2, 3, 4, 5].
- Ensure patients know of menstrual cups – while these still require vaginal insertion and may not be ideal for all patients, for some, these are significantly better than tampons as they require less frequent changing.
- Ensure patients are aware of the risk of toxic shock syndrome (TSS) that comes with keeping tampons in too long. Some may be more likely to keep a tampon in for an extended time because they are unaware of the risks or because they do not want to change their tampon in a public washroom [6].
- Ensure patients are aware of menstrual underwear (often advertised as “period underwear”) and other reusable menstrual products. Participants discussed a preference for period underwear as an ideal menstrual product (though many were initially unaware of its existence) [3].
- For example, Knix✝ offers a gender-neutral boyshort style underwear which has been advertised with trans model Sawyer DeVuyst
- Reusable products also reduce the frequency of buying menstrual products, which many participants found distressing [5].
- However, it should be noted that menstrual underwear is often cost-prohibitive and therefore may not be an appropriate suggestion for all patients.
- Ensure patients know of menstrual cups – while these still require vaginal insertion and may not be ideal for all patients, for some, these are significantly better than tampons as they require less frequent changing.
- There is an assumption within healthcare settings that all TNBGN people experience constant feelings of dysphoria and that all TNBGN people want to suppress their menstruation [7]. This is untrue, and to assume this of patients can be quite harmful and contribute to feelings of ‘not being trans enough’ [8]. Ensure you are actively listening to patients to understand their goals and their reasoning.
- TNBGN patients have often had to hide their gender identity from their doctors because of the assumptions healthcare providers make about how their gender influences their healthcare decisions [3,7]. For example, one non-binary participant was denied a hysterectomy to treat their endometriosis because the healthcare provider assumed they were using endometriosis as an excuse to “skip the line” for gender-affirming care [7].
- It is okay if you are unsure of how to provide gender-affirming care in the short-term; however, it is imperative that you know of appropriate practitioners to refer patients to.
- It can also be helpful to provide resources such as websites, community organizations, and support groups to refer patients to.
- While many healthcare providers remain relatively uneducated on how to provide gender-affirming care, patients must be able to connect with peers for two reasons.
- Being able to talk to other TNBGN menstruators helped participants re-frame their menses as less feminine, thus reducing their gender dysphoria [2].
- A network of TNBGN peers can help support proper gender-affirming treatment. For example, one participant described how they’d had a terrible experience using testosterone for gender-affirmation [7]. However, after talking to their peers, they learned it was likely they had been prescribed the wrong dosage. They then used their peers’ information to get their doctor to adjust the dose.
- Advocate for medical training to require training on caring for TNBGN patients.
Long-term Recommendations
- Attend formal training on how to care for TNBGN patients.
- Ensure you are properly educated on gender-affirming therapies before prescribing to patients.
- Note that testosterone is commonly mistaken as a contraceptive by both providers and patients when prescribed as part of gender-affirming care [9].
- While testosterone is commonly prescribed to suppress menstruation, know that it is not a guarantee. Many patients may require additional hormone therapy [9].
- Additionally, testosterone has teratogenic effects and can cause harm to any potential fetus [10]
- Note that non-binary and gender non-conforming patients (NBGN) may not want to use testosterone to suppress menstruation as they may not desire the masculine characteristics associated with testosterone [5]. Ensure other options are available.
- Note that people who identify as NBGN often find it more difficult to access care as they often feel unwelcome at clinics that cater specifically to women or specifically to trans patients [5].
- Note that testosterone is commonly mistaken as a contraceptive by both providers and patients when prescribed as part of gender-affirming care [9].
- When prescribing gender-affirming therapy, ensure you are also educating patients on the long-term effects of hormone therapies.
- Discuss how this may impact fertility and discuss the option for the preservation of gametes before starting treatment.
- Discuss how other medications or vaccinations may cause breakthrough bleeding after menstruation is initially suppressed [11].
- Discuss what patients can expect both in the short-term (how long it takes on average to stop menstruation, or if they will still experience cramps and mood swings) as well as long-term considerations (for example, how menopause will affect their menstruation and treatment).
With the above recommendations, I hope to help healthcare providers better understand the complexities of menstruation for TNBGN menstruators. Further, I hope to make clear that even small changes in practice, and an increased awareness of TNBGN care issues can result in significantly better care and health outcomes for TNBGN patients. That said, the academic literature on how TNBGN people experience and navigate menstruation is scarce. The existing studies are generally quite limited in their representation, focusing predominantly on young white participants. It is crucial to acknowledge that while the above recommendations may also be beneficial to older TNBGN patients, as well as Black, Indigenous, and people of the global majority (BIPGM) TNBGN patients, the recommendations are derived from studies that lack this diversity.
Read more here: https://doi.org/10.1080/13691058.2024.2375606
* I recognize that this term does not encompass the vast range of identities people in the population I am describing use to identify themselves. However, following the thoughtful guidance of a trans scholar, it is the term I deemed the most appropriate.
✝ Sex[M]ed does not endorse/oppose particular products without scoping review.
References:
1. Lane B, Perez-Brumer, A, Parker, R, Sprong, A, Sommer, M. Improving menstrual equity in the USA: perspectives from trans and non-binary people assigned female at birth and health care providers. Culture, Health & Sexuality. 2022;24(10):1408–22.
2. Chrisler JC, Gorman JA, Manion J, Murgo M, Barney A, Adams-Clark A. Queer periods: attitudes toward and experiences with menstruation in the masculine of centre and transgender community. Culture, Health & Sexuality. 2016;18(11):1238–50.
3. Frank SE. Queering menstruation: trans and non-binary identity and body politics. Sociological Inquiry. 2020;90(2):371–404.
4. Raynor G. Invisible menstruators: transgender and genderqueer individuals’ perceptions and experiences with menstruation [master’s thesis on the internet]. San Marcos (Texas): Texas State University; 2020 [cited 2023 Dec 12]. Available from: https://digital.library.txst.edu/server/api/core/bitstreams/4aec1ce6-d2d8-43ad-ac9e-7f401ab9b72f/content
5. Rydström K. Trans menstruators matter: a qualitative research exploring Swedish trans experiences with menstruation [master’s thesis on the internet]. Luleå (Norbotten County): Luleå University of Technology; 2018 [cited 2023 Dec 12]. Available from: https://www.researchgate.net/publication/351110516_Trans_Menstruators_Matter_A_Qualitative_Research_Exploring_Swedish_Trans_Experiences_with_Menstruation
6. Fahs B. The menstruating male body [Internet]. The Blood Project; 2016 [cited 2023 Dec 12]. Available from: https://www.thebloodproject.com/the-menstruating-male-body/
7. Lowik, AJ. “Just because I don’t bleed, doesn’t mean I don’t go through it”: expanding knowledge on trans and non-binary menstruators. International Journal of Transgender Health. 2021;22(1/2):113–25.
8. Kosher RBD, Houghton LC, Winkler IT. MANstruation: a cyberethnography of linguistic strategies of trans and nonbinary menstruators. Social Science & Medicine. 2023; 328:115974.
9. Roden, RC. Reversible interventions for menstrual management in adolescents and young adults with gender incongruence. Therapeutic Advances in Reproductive Health. 2023; 17:1-14.
10. Thornton KGS, Mattatall F. Pregnancy in transgender men. CMAJ. 2021 Aug 23;193(33):E1303. doi: 10.1503/cmaj.210013. PMID: 34426447; PMCID: PMC8412429.
11. Lee K, Junkins E, Clancy KP. Menstrual experiences after COVID-19 vaccination in a non-menstruating gender diverse sample. Poster session presented at: American Association for Anatomy; 2022 Apr 2-5; Philadelphia, United States. Available from: https://figshare.com/articles/poster/Poster_2022_American_Association_for_Anatomy_strong_Menstrual_experiences_after_COVID-19_vaccination_in_a_non-menstruating_gender_diverse_sample_strong_/22848734/1