Written by: Jaley Rae (she/her).
Edited by: Shelby MacGregor (she/her).
Period related disorders are often misunderstood, misdiagnosed, or their symptoms ignored or not believed. This lack of education around period related symptoms can lead to doctors not fully listening or providing the care we so desperately need. Many of us are told it is all in your head. Telling your doctor you want a second opinion, or you want to speak to a specialist, that you don’t agree with their diagnosis or treatment methods, or whatever else you need to do to advocate for the healthcare you deserve is an overwhelming task. Healthcare can be scary and traumatic and the stress of having to fight to be believed, to be taken seriously, and to be helped only adds to that trauma. This can be made worse if the doctors themselves do not fully understand the pain and discomfort you are experiencing.
I’ve felt this experience when trying to navigate the pain (both emotional and physical) I experienced around my period. “Maybe it’s just anxiety” was something I heard over and over until I wanted to burst. It can take a lot of strength and courage to be able to consistently self advocate for yourself and your healthcare. The power relations between patient and doctor can feel huge, especially since doctors often dictate the healthcare you receive. If a doctor is telling you nothing is wrong, then it can often feel like you are in a position where you do not have any right to argue with them. I had a doctor tell me that they thought a referral to a specialist was pointless; it was exhausting and discouraging. I needed an answer for why I was feeling such immense discomfort and pain. Why were my emotions going wild and severely disrupting my life 2 weeks before my period only to settle down and return to normal once I got my period?
“It’s just PMS, it’s normal” But I knew it wasn’t normal.
I knew the constant migraines, the disruptive mood swings, the severe breast pain, the chronic fatigue, muscle aches and pain, anxiety, depression, irritability, and sense of hopelessness was not a normal menstruation. I felt like my experience was being ignored and dismissed, like I was making it all up, and there wasn’t anything actually wrong with me despite what I was experiencing.
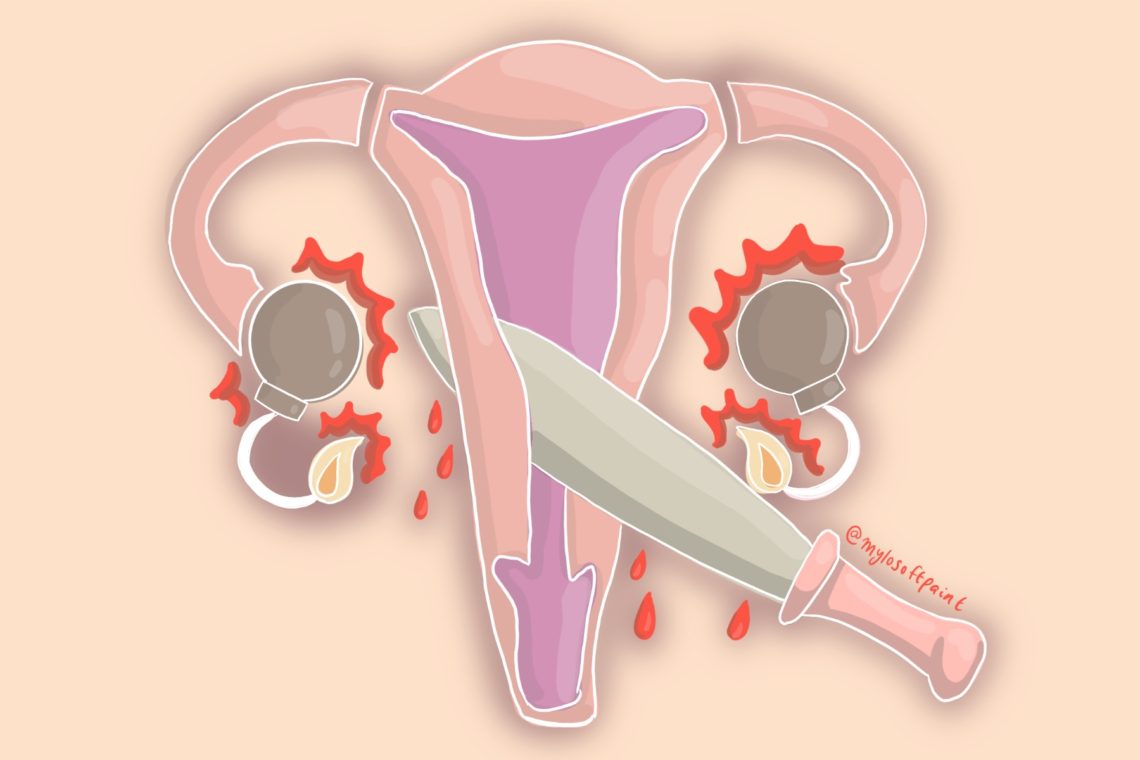
Since pain is subjective and there is no exact tool on how to measure pain, it can often be influenced by societal factors like gender norms. Often assumptions about gender norms are held by patients, researchers, and clinicians which leads to differences in treatment. If someone who is a women or femme and is experiencing something that is “medically unexplained”, their pain may be labeled a psychological issue or they can be perceived as hysterical, emotional, complaining, or fabricating the pain. It can take people a long time to meet a physician who believes them (1). We see this cycle happen continuously with period related disorders. Those who menstruate are reporting pain, emotional discomfort, and other unpleasant symptoms only for it to be dismissed or ignored (2). You don’t have to look too far to find articles reporting on people who claim their menstrual pain is not being believed. Period related disorders such as Endometriosis, PCOS, and PMDD are routinely missed due to healthcare professionals neglecting or ignoring the symptoms. This is compounded if there are intersecting systems of oppression such as race and sexuality (2).
If we look at PMDD, a lack of consensus and knowledge around the symptoms lead to PMDD being commonly misdiagnosed. PMDD is overlooked and research is underfunded with many believing it is nothing more than PMS. Even though it has severe symptoms both physical and mental and can affect up to 8% of people who menstruate, concerns are often dismissed within the healthcare system (3). The same is true for endometriosis and PCOS. Endometriosis is widely unknown even though it impacts roughly 1 in 10 women (the statistics for trans or gender non-binary persons are not known/represented in this study).
It can be incredibly difficult to get a diagnosis or even a referral to speak to a specialist – sometimes taking up to 7 years.
People are told the pain is normal despite the pain resulting in many trips to the hospital (4). PCOS unfortunately has the same patterns of pain and disbelief. There is a lack of awareness of PCOS causing physicians to not perform the necessary diagnostic tests or recognize the devastating consequences (5). PCOS can be horribly painful with side effects that deeply impact the patient’s daily life, yet their pain is going undiagnosed and ignored within the healthcare system (5).
All this to say, wherever you look, those who menstruate are having their pain and suffering ignored and prolonged because of a lack of education and awareness around these conditions within the health care system. Symptoms are overlooked, individuals are told it’s all in their head, and given “treatment” that is not right for what they are experiencing. Health care providers need to actively listen to patients when they are advocating for their menstrual needs. I finally did receive my referral and began working with a specialist, where I was diagnosed with Premenstrual Dysphoric Disorder (PMDD). Having the proper diagnosis meant I could access the treatment necessary for working with my condition. It meant having a proper explanation as to what was happening to me each month and validation for the pain I was experiencing. People deserve to have their experiences validated and their pain believed. It is not right that it can take years to find a proper diagnosis simply because healthcare providers refuse to acknowledge the validity of our symptoms. We know our bodies best and we have a right to advocate for our healthcare. I hope future healthcare providers learn more about period related disorders and the pain they cause and work to ensure people who menstruate are receiving the care and treatment they fundamentally deserve.
References:
1. Verge S. Doctors Ignored This Woman’s Suffering for Years. Why Is Women’s Pain So Often Dismissed? [Internet]. Reader’s Digest. Reader’s Digest; 2019 [cited 2021Feb22]. Available from: https://www.readersdigest.ca/health/conditions/womens-pain-undiagnosed/
2. Ro C. The overlooked condition that can trigger extreme behaviour [Internet]. BBC Future. BBC; 2019 [cited 2021Feb22]. Available from: https://www.bbc.com/future/article/20191213-pmdd-a-little-understood-and-often-misdiagnosed-condition
3. Landry J. She was in agony since age 13. Many didn’t believe her. Then a B.C. hospital diagnosed her with endometriosis | CBC News [Internet]. CBCnews. CBC/Radio Canada; 2021 [cited 2021Feb22]. Available from: https://www.cbc.ca/news/canada/british-columbia/endometriosis-lacking-research-1.5910342?fbclid=IwAR2QMfwUZBKcBjEcmTz7MBaIhVrRFCdPeBMi-3itwHqjz0X4v09rdv5memU
4. Parker S. The Common Hormonal Disorder That Scientists Don’t Understand [Internet]. The Atlantic. Atlantic Media Company; 2018 [cited 2021Feb22]. Available from: https://www.theatlantic.com/health/archive/2015/06/polycystic-ovary-syndrome-pcos/396116/